
#STEM CELL TREATMENT LUNG DISEASE TRIAL#
We propose the use of biomarkers that reflect clinically inconspicuous alterations of the disease molecular phenotype before rigid conclusions can be safely drawn. Signal Transduction and Targeted Therapy - The first human trial of CRISPR-based cell therapy clears safety concerns as new treatment for late-stage lung cancer Skip to main content Thank you for. Lung Disease The Scottsdale Stem Cell Treatment Center offers treatment for lung disease to residents of Scottsdale, Phoenix, and the surrounding Arizona communities. The mission in the Lung Program at the Cedars-Sinai Regenerative Medicine Institute is to use lung stem cells to identify critical determinants of lung.
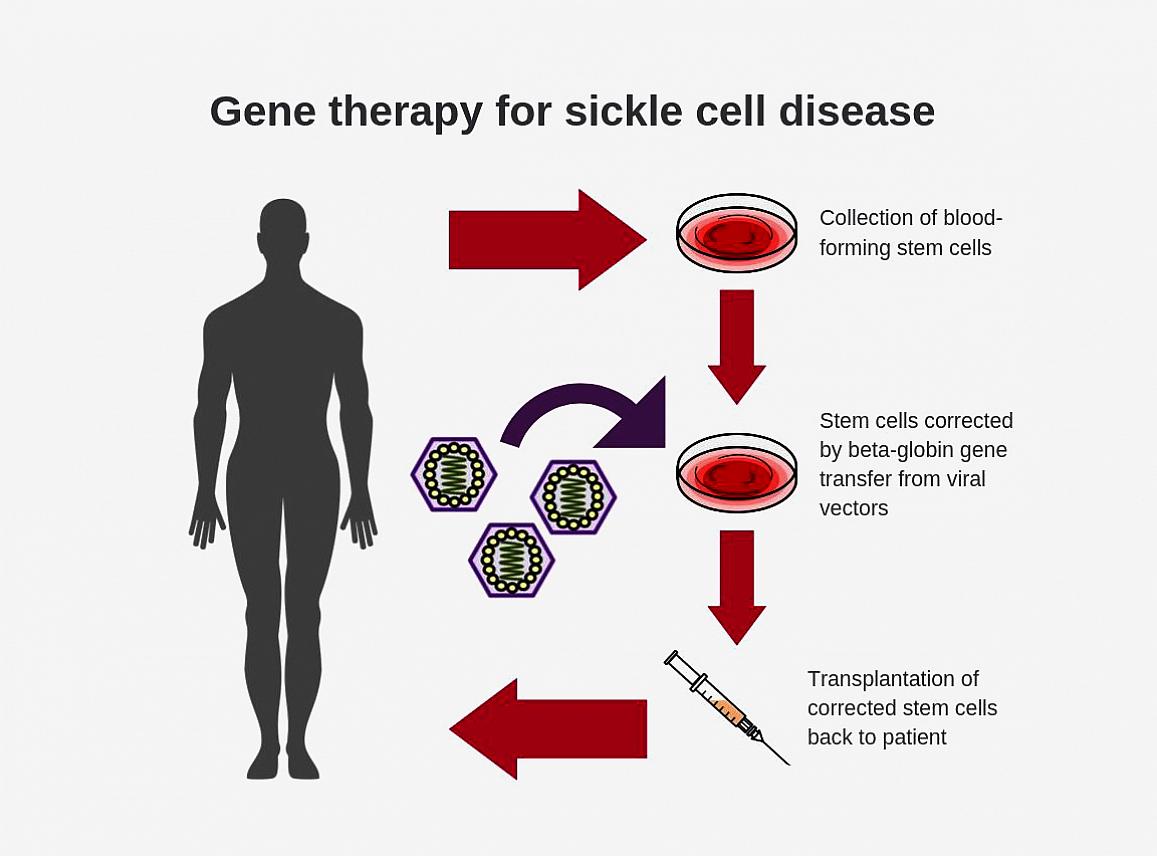
In this review, we argue in favor of large multicenter clinical trials setting realistic goals to assess treatment efficacy. The main scope of this review article is to summarize the current state of knowledge regarding the application status of stem cell treatment in chronic lung diseases, address important safety and efficacy issues and present future challenges and perspectives. On the other hand, salient data arising from few 'brave' pilot investigations of the safety of stem cell treatment in chronic lung diseases seem promising. Nevertheless, despite relative enthusiasm arising from experimental data, application of stem cell therapy in the clinical setting has been severely hampered by several safety concerns arising from the major lack of knowledge on the fate of exogenously administered stem cells within chronically injured lung as well as the mechanisms regulating the activation of resident progenitor cells. Regenerative medicine represents a promising option with several fruitful therapeutic applications in patients suffering from chronic lung diseases. We foresee the use of these MSC populations -alone or in conjunction with therapeutical molecules -as cell based therapy to treat chronic lung disorders. In view of the current disappointing status of available pharmaceutical agents, there is an urgent need for alternative more effective therapeutic approaches that will not only help to relieve patient symptoms but will also affect the natural course of the respective disease. This term is used very broadly to refer to a treatment involving the delivery of cells, obtained either from the person themselves or from a donor, to a diseased organ. Our hope is that discoveries and model systems established in this collaborative research will be broadly applicable to other distal airway diseases such as the spectrum of disorders seen in severe chronic obstructive pulmonary disease (COPD), cystic fibrosis and lung cancer.Chronic lung diseases such as idiopathic pulmonary fibrosis and cystic fibrosis or chronic obstructive pulmonary disease and asthma are leading causes of morbidity and mortality worldwide with a considerable human, societal and financial burden. It is this idea which invites the possibility that stem-cell therapy might be effective for lung disease.

Determine how intrinsic regulatory mechanisms that normally direct the fate of postnatal airway epithelial progenitors are reprogrammed in disease to assume inappropriate cell fates that lead to tissue remodeling.
#STEM CELL TREATMENT LUNG DISEASE HOW TO#
Define signals between epithelial progenitors and stromal cells that direct epithelial maintenance and repair in normal homeostasis and disease. To better understand how to effectively and consistently produce patient-specific iPS cells for lung-related clinical application, Mayo.Starting at ONLY 2950 for 30 million stem cells. As of now, there are no proven stem cell treatments for any lung disease, including COVID-19 and other respiratory infections from bacteria, viruses or fungi. The hypothesis is being tested in three specific ways: The mesenchymal stem cell therapies are performed with umbilical cord derived biologics that exceed FDA regulatory standards, and R3 has never experienced a significant adverse event. A stem cell treatment that restores lung cell function might be able to reverse or even cure some lung diseases. Exogenous mesenchymal stem cells (MSCs) have been reported to repair the structure and improve the function of the injured respiratory system in COPD models. The research team is currently testing the hypothesis that epithelial progenitors receive environmental and intracellular signals that are essential for normal homeostasis and injury repair, and that these cells are dysregulated in lung disease. The Lung Program, based in the lab of Barry Stripp, PhD, is collaborating with Paul Noble, MD, chair of the Department of Medicine Clive Svendsen, PhD, director of the Regenerative Medicine Institute and Moshe Arditi, MD, director of Pediatric Infectious Diseases.


 0 kommentar(er)
0 kommentar(er)
